Scientific Update
Background
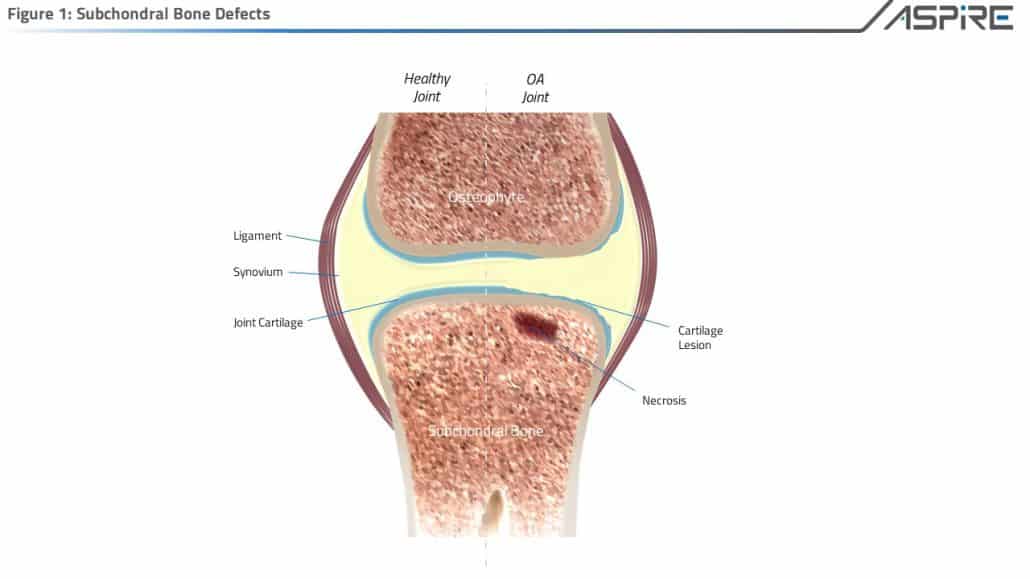
Unfortunately, damage to cartilage is not readily repaired by the body. That’s because cartilage unlike most tissues in the body doesn’t have its own blood supply to bathe damaged tissue and provide factors promoting regeneration.
Treating cartilage and subchondral bone defects typically encompass both biologic as well as structural components.
- Biological aspects typically include: Marrow Stimulation efforts such as, K-Wire Drilling, Micro-Fracturing, Nano-Fracturing, Core Decompression or additive therapies such as autologous PRP Injections, Adipose derivations, and Bone Marrow Cell Injections.
- Subchondroplasty aspects range from Cement Injections, Allograft Transplantation, ACI Procedures, Bone Marrow Cell Graft Injections, Iliac Crest (Tibia) Bone Grafting options.
Osteo-Core-Plasty™ with Marrow Cellution™ provides both Biologic and Structural components to provide an optimized environment for regeneration.
Bone remodelling is a dynamic process that involves a combination of an osteoconductive functional matrix, living cells that produce osteoinductive growth factors and osteogenetic cells that form new bone.
Autograft is defined as bone tissue transferred from one site to another in the same individual. Autograft has traditionally been the gold standard in bone grafting because it is proven and predictable.
Autograft is an osteoconductive matrix and works because:
- Cells are harvested with the transplanted matrix structure.
- Cells can migrate within the transplanted matrix from the peripheral blood infrastructure.
- Cells can mobilize from the marrow space and home to the transplanted matrix (i.e. vasculogenesis) drive osteoinduction and osteogenesis.
Commonly employed types of autograft are derived from the Iliac crest and Tibial plateau.
Normal physiologic bone healing undergoes a cascade of three overlapping phases:
- Hemostasis & Inflammation
- Proliferation
- Remodelling
Autophagy is a cellular housekeeping mechanism that is responsible for the removal of necrotic tissue, dead cells, neutrophils and dysfunctional intracellular proteins. Autophagy occurs during the inflammation phase of healing. (1)
Experiments demonstrate that the flow of blood through compact bone depends predominantly on an intact blood supply from the marrow. In living bone, unimpaired microcirculation is indispensable for the viability of bone cells, the production of new bone substance, and the regulation of bone metabolism. (2,3)
Morselized Bone compared to Intact Bone
Bones are dynamic, viable, highly organized living tissue. Autologous cancellous bone pieces are osteoconductive, osteoinductive and osteogenic.
Traditional harvesting of autograft typically requires a soft tissue cut down technique and creation of a fenestration of the cortical bone complex to gain access to the cancellous marrow cavity. This open process of collecting small pieces of cancellous bone dramatically increases pain and morbidity for the patient as well as, disrupts the highly organized structure and supporting microvasculature of bone.
Combination Bone Grafts
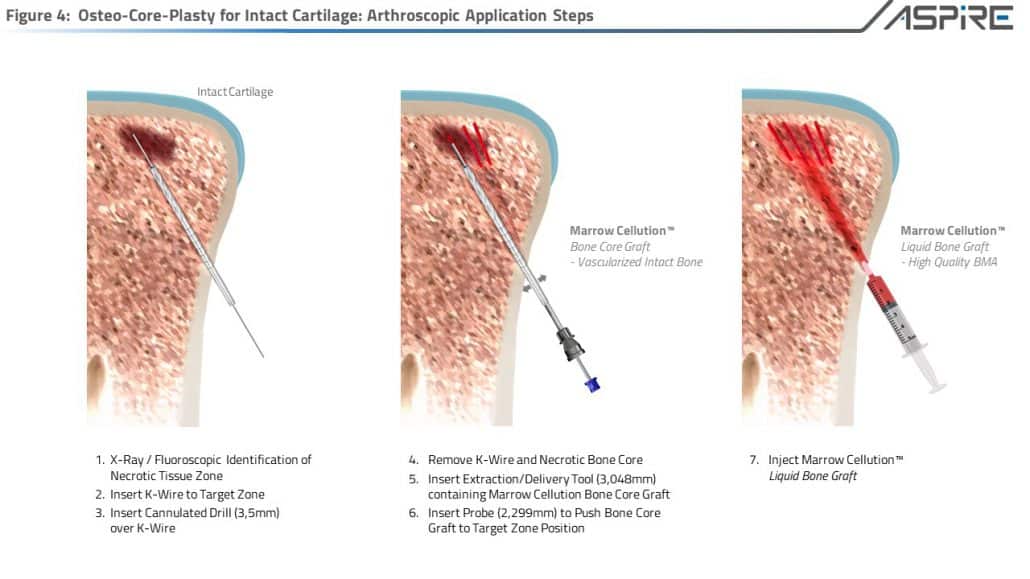
Vascularized and cancellous autograft show optimal skeletal incorporation but are limited by morbidity concerns. (4) The percutaneous utilization of the Marrow Cellution graft delivery syringe and the Marrow Cellution Bone Dowel Harvest device, the clinician can create a combination graft of a vascularized intact bone dowel in the center of the graft surrounded by allogeneic, autologous or synthetic bone chips hydrated with marrow aspirate.
These grafts heal by means of creeping substitution. Transplanted and migrating cells drive peripheral and internal resorption by removing the transplanted matrix over time through the process of autophagy. Subsequently, during the remodelling phase, cells form a callus in place of the resorbed tissue and then structured living bone. (2,3) Harvesting an intact cancellous bone core dowel which does not disrupt the highly-organized living tissue of the bone is different from transplanting pieces of bone. Such grafts that maintain the micro-vascular within the graft do not show extensive resorption, callus formation or remodelling. (2,3) The inherent difference is based on the ability of intact bone to exploit the biology of normal fracture healing rather than through creeping substitution that is fundamental to the incorporation of a non-vascularized graft. (2)
Research demonstrates the enhanced survival of a free bone graft as long as its primary blood supply is preserved or re-constituted. A living bone graft will shorten the time to heal because the reconstructed bone is comparable to a bone with a double fracture. (2,3) Allogeneic or synthetic bone chips hydrated with marrow can be packed around the living bone graft/dowel to accelerate anastomosis into the graft and minimize the amount of morbidity. (2,3)
Osteo-Core-Plasty™
The Marrow Cellution™ Osteo-Core-Plasty™ is a X-Ray or fluoroscopic guided, minimally invasive, autologous, biologic procedure that allows for necrotic bone segment resection and transplants living, vital, intact bone core segments that have the capacity to reincorporate naturally without foreign body implantation.