What are the limitations of traditional trocar needles and what is the optimal technique for minimizing peripheral blood dilution?
Optimal technique for minimizing peripheral blood with a traditional aspiration needle is to perform a single small volume pull (1-2 mL) from the distance most proximal from the entry of the needle. Larger volumes of bone marrow aspirate contain higher amounts of peripheral blood because the cannula is open ended and because traditional needles do not have a mechanical means for precise relocation. Aspirating after retracting the needle exacerbates the problem of peripheral blood collection by exposing the open ended cannula to the resulting channel that is created by the needle itself and that is filled with peripheral blood.
Strict adherence to a specific collection procedure, involving small volume marrow aspirations and multiple puncture sites, results in a product with a high number of early hematopoietic progenitor cells and minimal contamination by peripheral blood.1
As the aspiration volume increases from any one given site, the concentration of bone marrow derived cells decreases quickly and the fraction of the sample composed of peripheral blood increases.2
Marrow harvesting by means of multiple small volume aspirations minimizes the dilution with peripheral blood and results in greater numbers of cells and hemopoietic progenitors.3
Aspirates of bone marrow demonstrated greater concentrations of mesenchymal stem cells with a 10-ml syringe compared with matched controls using a 50-ml syringe.4
A larger-volume of aspirate from a given site is contraindicated with the additional volume contributing little to the overall number of bone-marrow cells and results principally in unnecessary blood loss.2
(1) Spitzer TR, et al. The impact of harvest center on quality of marrows collected from unrelated donors. J Hematother. 1994 Spring;3(1):65-70.
(2) Muschler GF, et al. Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume. J Bone Joint Surg Am. 1997 Nov;79(11):1699-709.
(3) Bacigalupo A, et al. Bone marrow harvest for marrow transplantation: effect of multiple small (2 ml) or large (20 ml) aspirates. Bone Marrow Transplant. 1992 Jun;9(6):467-70.
(4) Hernigou P, et al. Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells. Int Orthop. 2013 Nov;37 (11): 2279-87.
Does a small volume aspirate have more CFU-f than a larger draw that is then volume reduced by centrifugation?
IIn order to centrifuge marrow, you need to add 10% by volume anti-coagulant. This dilutes the end product. You do not need to add that volume of anti-coagulant if you are not centrifuging.
When you centrifuge marrow, approximately 40% of the stem cells are discarded with the red cells. Stem cells / progenitor cells when they are cycling build up nucleic mass prior to division. At this stage their density increases dramatically to the point where they have a similar density to a red cell. Centrifugation protocols capture a range of cells based on density. In any given aspirate, approximately 40% of the stem cells have density outside what is typically captured in the buffy coat.
Typically, the centrifugation protocol volume reduces the aspirate from 60mL to 10mL. This 10mL is then used to hydrate the substrate. However, in order to reverse the effect of the anti-coagulant, to make the marrow clot, about 1mL of calcium chloride and thrombin is mixed with the concentrate – another 10% dilution.
Centrifuge does not distinguish between nucleated cell from marrow versus blood. So, a sample may have a lot of nucleated cells but very few came from marrow. A CFU-f test is often performed on marrow aspirate because CFU-f are found in marrow but not blood.
Finally, there is no way to draw 60mL of marrow, no matter how careful, and not get significant peripheral blood dilution. A careful draw of 60mL with multiple punctures typically, at best, gets on average 300 CFU-f per mL.
The math play for a typical centrifuged marrow aspirate sample plays out as follows:
Total aspiration volume: 60mL
CFU-f per mL: 300
Total no. of CFU-f: 18.000
Recovery in Concentrate: 60% –> Total CFU-f in Concentrate: 10.800
Concentrate Volume: 7mL –> CFU-f per mL: 1.543 (HSS/Hedge Study: 1.270)
This compares to approx. 2.000 CFU-f per mL drawn from a single site in the marrow.
Juopperi TA, et al. Isolation of bone marrow-derived stem cells using density-gradient separation. Exp Hematol. 2007 Feb;35(2):335-41.
Bhartiya D, et al. Very small embryonic-like stem cells with maximum regenerative potential get discarded during cord blood banking and bone marrow processing for autologous stem cell therapy. Stem Cells Dev. 2012 Jan;21(1):1-6.
Vishal Hegde MD, et al. A prospective comparison of three approved systems for autologous bone marrow concentration demonstrated non-equivalency in progenitor cell number and concentration. J Orthop Trauma. 2014 Oct;28(10):591-8.
Muschler GF, et al. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am. 1997 Nov;79(11):1699-709
Hernigou P, et al. Benefits of small volume and small syringe for bone marrow aspirations of mesenchymal stem cells. Int Orthop. 2013 Nov;37(11):2279-87.
What is the relationship between age and aspiration quality for bone marrow?
- The cellularity of marrow declines with age
- The cellularity of marrow per mL declines with increasing aspiration volumes.
Muschler G, et al. Age- and gender-related changes in the cellularity of human bone marrow and the prevalence of osteoblastic progenitors. J Orthop Res. 2001 Jan;19(1):117-25.
Pang WW, et al. Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age. PNAS 2011, vol. 108 no. 50, 20012-20017
What is the importance of CFU-f counts compared to Nucleated Cell counts?
There is no constant ratio between average marrow cellularity as measured by number of total nucleated cells per mL and the number of Colony-forming unit fibroblast (CFU-f). Hernigou et al in several authoritative studies linked clinical outcomes in non-union and osteonecrosis to the number of CFU-f cells in the graft. Controlling for volume, Hernigou noted that 70% of the variation in CFU-f from patient to patient was due to variations in the quality of the marrow aspirate or idiosyncratic to the patient with the remaining variation being due to the number of nucleated cells per mL in the aspirate. Statistically, the only variable Hernigou reported to be significant was CFU-f and not nucleated cells per mL. Interestingly, CFU-f is found frequently in marrow and very rarely in peripheral blood.
Therefore, it seems reasonable to suggest that a graft needs to contain greater than 1000 progenitors/cm³
Hernigou P, et al. Treatment of Osteonecrosis with autologous bone marrow grafting. Clinical Orthopaedics and Related Research. 405:14-23, 2002.
Hernigou P, et al. Percutaneous Autologous Bone-Marrow Grafting for Nonunions – Influence of the Number and Concentration of Progenitor Cells. J Bone Joint Surg Am. 2005 Jul;87(7):1430-7.
What is the importance of CD34 compared to Nucleated Cell counts?
The hematopoietic colony-forming cell content of the transplant is associated more rigorously with the major covariates of success than is the total nucleated cells and is, therefore, a better index of the content of grafts.
Migliaccio AR, et al. Cell dose and speed of engraftment in placental/umbilical cord blood transplantation: graft progenitor cell content is a better predictor than nucleated cell quantity. Blood. 2000 Oct 15;96(8):2717-22.
What is the role of Red Cells in tissue regeneration?
Red Cells are a natural part of any clot and play a role in the regenerative process; it is not necessary to remove them.
- Red Cells are nitric oxide sinks1
- Nitric Oxide is a potent stem cell stimulant2
- Red Cells release iron
- Iron is used by cells under stress to survive and function3
- Stem cells reside deep in the Red Cell layer, all centrifuge based protocols discard the Red Cell layer under the buffy coat4,5,6
The isolated cells from both the upper and lower fractions were characteristic of MSC. Although it is commonly believed that MSC are single suspending mononuclear cells and so are enchriched in the upper fraction of Ficoll-Paque after density-gradient separation, our data showed that considerable numbers of these cells were accumulated in the lower fraction.4
(1) Cortese et al Endothelial nitric oxide synthase in red blood cells: Key to a new erythrocrine function Volume 2, 2014 251-258 http://www.sciencedirect.com/science/article/pii/S221323171400010X
(2) Alexandra Aicher Essential role of endothelial nitric oxide synthase for mobilization of stem and progenitor cells Nature Medicine 9, 1370 – 1376 (2003) Published online: 12 October 2003
(3) Gardner, et al Superoxide Radical and Iron Modulate Aconitase Activity in Mammalian Cells June 2, 1995 The Journal of Biological Chemistry, 270
(4) Ahmadbeigi et al The aggregate nature of human mesenchymal stromal cells in native bone marrow. Cytotherpy 2012 Sep;14(8):917-24.
(5) Juopperi et al Isolation of Bone Marrow Derived Stem Cells using Density-Gradient Separation Experimental Hematology 35 (2007) 335-341
(6) Bhartiva D et al “Very Small Embryonic-Like Stem Cells with Maximum Regenerative Potential Get Discarded During Cord Blood Banking and Bone Marrow Processing for Autologous Stem Cell Therapy” Stem Cells and Development Volume 221 NO 1 2012
Is there a relationship between differing volumes of bone marrow aspirates and their cellular composition?
A dramatic decline in the number of HSC and CFU-f is observed with increasing amounts of marrow aspiration. With respect to HSC and in the setting of large volume aspirations (1,000 mL and greater) for allogeneic transplantation, the first 1mL of marrow had 3X (300%) more nucleated cells and 10X (1000%) more stem cells than the overall aspirate. Similarly, it has been documented that the number of MSC per/mL significantly decreases with increased volumes of aspirate taken. The table below demonstrates this phenomena by comparing the number of CFU-f per mL in differing volumes of aspirate in similar patient populations:
| Volume of Aspirate: | 1 mL | 10 mL | 55 mL |
| CFU-f/mL: | 1458 | 675 | 254 |
Importantly, the number of CFU-f in incremental aspirations of over 100 mL have as little as 60 CFU-f / mL.
Batinic D, et al. Relationship between differing volumes of bone marrow aspirates and their cellular composition. Bone Marrow Transplant. 1990 Aug;6(2):103-7.
Li J, et al. Factors Affecting Mesenchymal Stromal Cells Yield from Bone Marrow Aspiration. Chin J Cancer Res. 2011 Mar;23(1):43-8.
Muschler GF, et al. Aspiration to Obtain Osteoblast Progenitor Cells from Human Bone Marrow: The Influence of Aspiration Volume. J Bone Joint Surg Am. 1997 Nov;79(11):1699-709.
Hegde V, et al. A prospective comparison of three approved systems for autologous bone marrow concentration demonstrated non-equivalency in progenitor cell number and concentration. J Orthop Trauma. 2014 Oct;28(10):591-8.
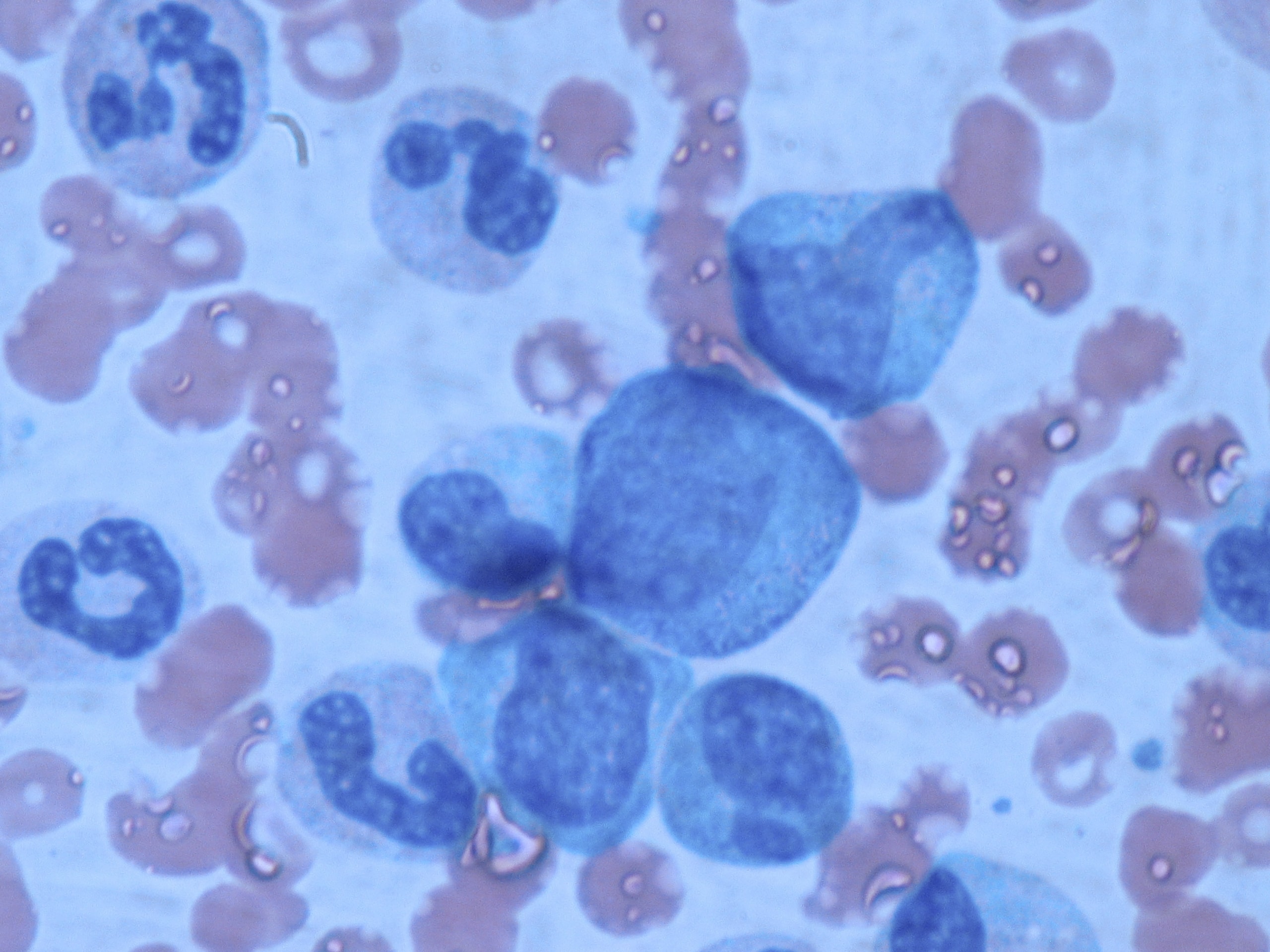
What are TNC, MNC, CD34+, and CFU?
Stem cells happen to be Mono-Nuclear Cells or MNC: when you look at them under a microscope there is only one nucleus. Unfortunately, one of the most difficult aspects of stem cell biology is that you can’t identify a stem cell just by looking at it. There are other types of cells which are also MNC, such as nucleated red blood cells. The only proof that a cell is a stem cell comes from how it behaves when it multiplies.
Scientists have worked for years to develop various chemical stains which have a high affinity for stem cells. The best known marker for stem cells is that they test positive for CD34, a protein found on the surface of stem cells. But, CD34+ counts are not an accurate measurement: CD34+ results vary between labs, they can vary within a single lab, and only 1-2% of the MNC that have CD34+ are actually stem cells.
The Total Nucleated Cell count or TNC is the test most often reported as a measure of the cell count after processing. The main advantage of measuring TNC is that the count is highly reproducible within and among labs. Even better, the TNC count can be automated with the use of a device called a flow cytometer.
At present Colony Forming Units or CFU are considered to be the best measure of whether stem cells are “viable”, or quite frankly alive. The TNC count includes both living and dead cells. In the CFU test a small portion is watched under controlled conditions to see if stem cells divide and form colonies. This used to be a subjective measure, but recently it has been standardized with technology to image the cells and count colonies in the image. The only remaining problem with the test is that it takes days for colonies to grow.
What is the purpose of centrifugation protocols for marrow?
To compensate for peripheral blood dilution due to with increasing volumes of aspiration from a single location within the marrow space, clinicians have used centrifugation protocols to volume reduce 50 to 60 mL of aspirate to 7 to 10 mL by removing excess plasma and red blood cells from the peripheral blood. The final treating composition typically has a concentration above baseline of nucleated cells from the peripheral blood and the marrow.
Muschler GF, et al. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am. 1997 Nov;79(11):1699-709.
Hegde V, et al. A prospective comparison of 3 approved systems for autologous bone marrow concentration demonstrated nonequivalency in progenitor cell number and concentration. J Orthop Trauma. 2014 Oct;28(10):591-8.
What is the impact of age on peripheral blood platelets, and vasculogenesis?
Platelets and white blood cells from peripheral blood are essential to healing and the body naturally aggregates platelets and white cells efficiently to sites of trauma. With age, your body does not lose its ability to aggregate platelets from blood to the area of a defect. Vasculogenesis (i.e. the ability of your body to mobilize stem cells from the marrow space to the site of trauma) does diminish significantly with age because of fewer stem cells in the body and a diminished ability to travel to sites of a defect. With age, marrow mediated healing diminishes dramatically.
Transplanting marrow exactly at the site of injury mimics and supplements your body’s critical response to healing, a response that diminishes with age.
Lommatzsch M, et al. The impact of age, weight and gender on BDNF levels in human platelets and plasma. Neurobiol Aging. 2005 Jan;26(1):115-23.
Heiss C, et al. Impaired progenitor cell activity in age-related endothelial dysfunction. J Am Coll Cardiol. 2005 May 3;45(9):1441-8.
Scheubel RJ, et al. Age-dependent depression in circulating endothelial progenitor cells in patients undergoing coronary artery bypass grafting. J Am Coll Cardiol. 2003 Dec 17;42(12):2073-80.
Do certain diseases impact the number and or functionality of CD34+ cells & CFU-f in the marrow?
Sickle cell disease and diabetes are known to impact the marrow space. In the case of sickle cell disease, the marrow space tends to be hyper-active and marrow aspirates from these patients are associated with higher numbers of CD 34 and CFU-f.
In the case of diabetes, the functionality of the marrow cells is significantly impaired.
Hernigou P, et al. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23.
Tepper OM, et al. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation. 2002 Nov 26;106(22):2781-6.
Do certain medications impact the number of CD34+ cells & CFU-f in the marrow?
Amongst others:
Statins are associated with a dramatic and dose dependent increase in the number of CD34 cells in both the marrow and in circulation.
Corticosteriod use is associated with impaired cellularity of the marrow space and osteonecrosis of the hip.
Bisphosphanate use is associated with osteonecrosis of the jaw.
Dimmeler S, et al. HMG-CoA reductase inhibitors (statins) increase endothelial progenitor cells via the PI 3-kinase/Akt pathway. J Clin Invest. 2001 Aug;108(3):391-7.
Hernigou P, et al. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23.
Marx RE, et al. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005 Nov;63(11):1567-75.
Do certain lifestyle choices impact the number of CD34+ cells & CFU-f in the marrow?
Conditions such as alcohol abuse, smoking, lack of exercise and a poor diet are associated with fewer numbers of CD34+ cells and CFU-f in the marrow.
Hernigou P, et al. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002 Dec;(405):14-23.
Mackie AR, et al. CD34-positive stem cells: in the treatment of heart and vascular disease in human beings. Tex Heart Inst J. 2011;38(5):474-85.
FAQ did not solve your problem?
Here are several ways to contact us
Need Support?
Please use our Contact page to get in touch.
Check Our Intranet-Website
(login required)